Australian doctors designing their own PPE due to limited supply
Share
Australian doctors who are worried the system won’t be ready to provide them with the equipment they have to guard themselves and their patients during the COVID-19 pandemic are watching ways to style and produce their own.
Doctors are concerned about the supply of apparatus to guard both themselves and patients, one Melbourne anaesthetist, who wished to stay anonymous, told the ABC.
“Many doctors and health professionals are very concerned and confused about the wants for, and current supply of, personal protective equipment (PPE) for hospitals,” she said.
“Some hospitals now have but one week of accessible stock of this kind of apparatus to cope with any potential or known COVID-positive patients.
“This situation is applicable to normal or emergency surgery, emergency rooms and inpatient ward care, yet because the treatment of COVID-positive patients.”
A large centralised group involving Victorian university staff, clinicians and makers has been working tirelessly to develop suitable products and to co-ordinate the provision and demand of those essential items, and it’s begun to network with other similar groups across Australia and internationally.
hey have reached bent philanthropic organisations and native engineers and makers to open up supply lines and located them keen to assist.
The PPE items they’re working to form so as to cut back the chance to staff and secure their safety include:
- Face shields
- Hooded oxygen respirators for both patients and staff to guard from airborne exposure
PPE masks with viral filters - Clear anaesthesia “splash boxes” for intubation
- Rapid portable CPAP (continuous positive airway pressure) devices for home patients needing increased support for ventilation
- Ventilators and ventilator parts or “splitters” to enable one machine to support two patients’ breathing
On top of the doctors’ efforts, a Department of Health and Human Services (DHHS) task force has been established to assess this dynamic supply and demand situation, while the department of the federal government of Industry, Science, Energy and Resources has founded a ventilator task force.
Con Kolivas, a retired anaesthetist and coder who helps to coordinate one in all the groups, said it started as an informal chat between some people about the shortage of ventilators in Italy at the time.
They wondered whether it’d be possible for Australia to create some quite simple ventilator just in case of a shortage locally.
“The rate of infection of medical staff within the worst-affected areas overseas is now very high and, to create matters worse, doctors who’ve been infected at the line appear to possess the next death rate than people who’ve caught it within the community,” he said.
“I et al approached people from different disciplines in industry, medicine, engineering, software then on about what we could do and located a cohort of individuals willing to assist out.
“After the initial discussion about ventilators, talks turned to things we could manufacture locally and private protective equipment (PPE) was top of the list.
“This is an infection that we’ve never faced before so we need novel approaches to things.
“Government and health suppliers don’t actually give us any of this type of kit, so we would have liked to innovate because there’s not a straightforward path to search out these novel pieces of kit.””The whole world is trying to accumulate the identical resources at the identical time and that we are falling into the rest room roll trap,” Dr Ilancheran said.
“Our group feels is it imperative that we source local engineers and makers to still have the availability chain of the essential equipment that we want to avoid wasting lives during this pandemic.
“We are aware that because the lockdown phase gets stricter, we are going to have further supply chain issues.”
Dr Kolivas said the Victorian Government was keen to support any firm designs the group could come up with, except for any complex designs, the regular government channels of approval and funding could slow things down.
Fortunately, various philanthropical organisations were also very willing to help, he said.
“With the assistance of 3D printing it makes it possible to tackle any reasonably design we wish,” Dr Kolivas said.
“The problem with 3D printing is it’s slow, so it’s great for producing the prototypes, but you cannot mass produce them if every one takes two hours to print.”
That is where support from local manufacturers comes in.
Dr Kolivas said that, again, there was a desire to assist.
Toyota is one example of a corporation which has offered its design and engineering capabilities to provide equipment on an oversized scale.
Crucially, Dr Kolivas said, ventilator manufacturer Medtronic had displayed one in every of its designs at no cost use during the pandemic, without property restrictions, meaning there was potential for manufacturers to provide the vital piece of kit in Australia.
A website, COVID SOS, has been founded as a central hub for the varied groups out there acting on novel solutions.
It is also trying to handle frontline medical equipment shortages through community-sourced methods of design and manufacture.
Here are some samples of the equipment the group is functioning on:
Intubation Boxes
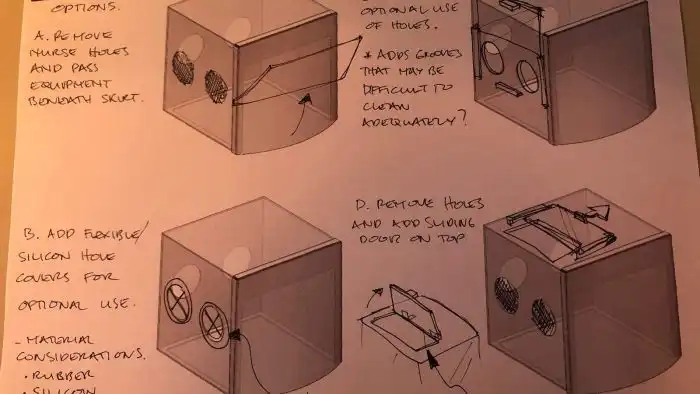
Dr Kolivas:
“The “intubation box” is an example of an alternative novel PPE to deal with the unique threat of coronavirus.
When a patient is so severely affected by the respiratory complications that they need to be put on a ventilator, they need to have a tube put into their trachea to connect them up to the ventilator.
That particular procedure puts the doctor (usually an anaesthetist, intensive care specialist, or emergency physician) and assisting staff in very close proximity with the patient’s respiratory tract — they’re literally staring down the patient’s throat.
The potential for aerosol exposure there is extreme, and our clinicians had seen perspex shells used overseas for that scenario to limit that exposure.
We developed our own solution, as you can see in the diagram, where the patient is under perspex with rubber-like seals to drop around the patient, and it has self-sealing hand holes for the clinicians to do their intubation.
The design was revised and simplified a few times and is made from laser-cut perspex, so is ultimately not that complex to build, which is important. It has been tested clinically with success already and we’re looking to produce a number of these for multiple hospitals.”
Face Shields

Dr Kolivas:
“The facial shield is a very simple guard to/from the staff member which provides an impermeable barrier to any aerosols being sprayed in either direction.
It obviously doesn’t provide a perfect airtight seal but it affords a great deal of confidence when performing procedures on infected patients.
We were able to prototype these from an open-source design on the internet and 3D print them.
3D printing has allowed us to rapidly get a design built, so it allows for rapid prototyping, but is very slow in production.
A local manufacturer has taken up the need for facial shield designs and has said they’ll be able to produce them in the thousands.
We have been connecting hospital networks with this manufacturer to allow them to test out their prototypes and they should be able to order them immediately.”
Ventilation Splitters

“The ventilator splitter is a simple three-way hard piece of tubing. With the potential for running out of ventilators being very real, the splitter gives us a means to use one ventilator on multiple patients instead of the one person which it’s normally designed for.
It’s a use that ventilators were never approved for, and we have not used them in that manner locally, nor do they work ideally in such circumstances.
However, it effectively doubles the capacity of ventilators we have should we run out due to the demand, and allows us to keep using sophisticated ventilators to manage patients, instead of trying to use a much simpler and riskier “bag squeezing” design that would be more in keeping with third-world life-saving emergencies.”
Oxygen Hoods

Photo: Oxygen Hood (from Amron)
“The oxygen hoods we’ve been looking at are a tent that sits over a person’s head that allows us to use higher oxygen concentrations in a closed system than the usual “oxygen masks” that are used in abundance in hospitals.
Regular oxygen masks vent all their excess gas back into the room and have practical upper limits to the inspired oxygen concentration they provide.
The higher the oxygen concentration we are able to administer, the less likely a patient is to require to be intubated and ventilated.
A commercial manufacturer of these has given permission for local manufacturers to build these without intellectual property issues.”












